Understanding Tonsil Grading: What You Need to Know
Have you ever wondered about the size of your tonsils or your child’s tonsils and what it means? Tonsil grading is a standardized method healthcare professionals use to assess and document tonsil size. It’s a crucial part of understanding potential airway obstruction and related health issues. This comprehensive guide will take you through everything you need to know about tonsil grading, from its basic principles to its clinical significance, providing you with the knowledge to understand this important assessment and its implications for your health.
The Fundamentals of Tonsil Grading
Tonsil grading is a visual assessment performed during a physical examination. It aims to quantify the extent to which the tonsils occupy the oropharynx (the back of the throat). This assessment is primarily subjective, relying on the examiner’s judgment, but standardized grading systems help ensure consistency and accuracy.
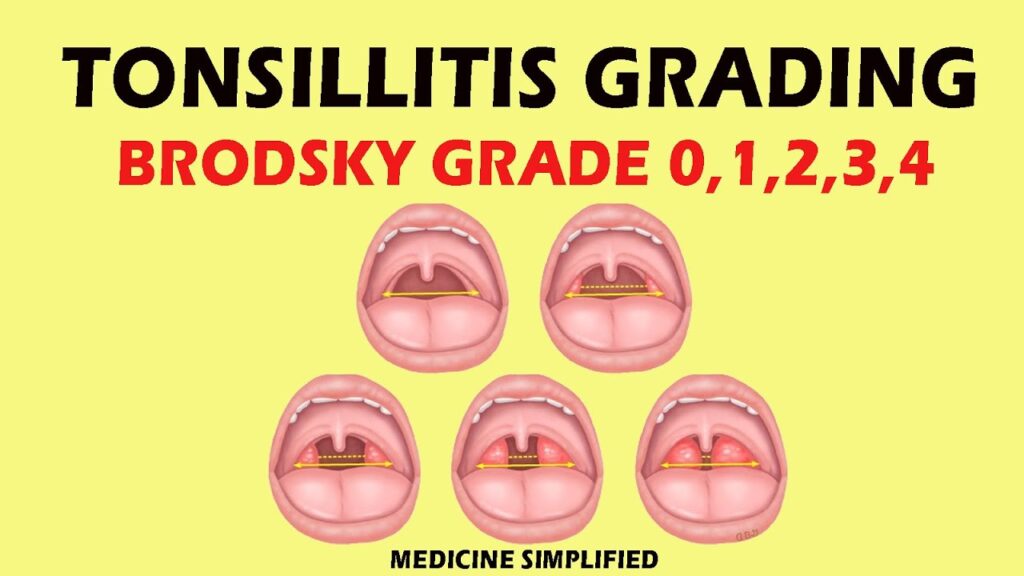
The most commonly used grading scale ranges from 0 to 4:
- Grade 0: Tonsils are entirely within the tonsillar fossa (removed).
- Grade 1: Tonsils are hidden behind the tonsillar pillars (the folds of tissue in front of the tonsils).
- Grade 2: Tonsils extend to the tonsillar pillars.
- Grade 3: Tonsils extend beyond the pillars but do not touch the uvula.
- Grade 4: Tonsils extend to or beyond the midline, potentially touching each other (kissing tonsils).
It’s important to note that “normal” tonsil size varies among individuals and age groups. Children, for example, often have larger tonsils than adults. A high tonsil grade doesn’t automatically indicate a problem, but it can be a contributing factor to certain conditions.
The History and Evolution of Tonsil Grading
The concept of tonsil grading has been around for decades, evolving alongside our understanding of airway obstruction and related conditions. Early methods were less standardized, leading to inconsistencies in assessment. The development of the 0-4 scale provided a more uniform approach, facilitating better communication among healthcare providers and more reliable tracking of tonsil size over time. Ongoing research continues to refine our understanding of the clinical significance of different tonsil grades.
Why Tonsil Grading Matters
Tonsil grading is essential because enlarged tonsils can contribute to various health issues, particularly in children. These include:
- Obstructive Sleep Apnea (OSA): Enlarged tonsils can obstruct the airway during sleep, leading to pauses in breathing.
- Snoring: Tonsil size is a significant factor in snoring, although not all snorers have enlarged tonsils.
- Difficulty Swallowing (Dysphagia): Very large tonsils can make it difficult to swallow food.
- Recurrent Tonsillitis: While not directly related to size, enlarged tonsils can sometimes contribute to more frequent infections.
Accurate tonsil grading helps healthcare providers assess the severity of these conditions and determine the most appropriate course of treatment.
The Role of Endoscopy in Tonsil Evaluation
While visual examination remains the primary method for tonsil grading, endoscopy offers a complementary approach. Endoscopy involves using a small, flexible camera to visualize the upper airway, including the tonsils. This can be particularly useful in cases where the tonsils are difficult to visualize due to their position or other anatomical factors. Endoscopy can also help assess the degree of airway obstruction more accurately than visual examination alone.
Benefits of Endoscopic Tonsil Evaluation
- Improved Visualization: Endoscopy provides a clearer and more detailed view of the tonsils and surrounding structures.
- Accurate Assessment of Airway Obstruction: Endoscopy can help determine the extent to which the tonsils are obstructing the airway.
- Detection of Underlying Conditions: Endoscopy can help identify other potential causes of airway obstruction, such as nasal polyps or a deviated septum.
Endoscopy is typically performed by an otolaryngologist (ENT specialist) and is a relatively quick and painless procedure.
Detailed Feature Analysis of Tonsil Grading
Tonsil grading isn’t a complex procedure, but its value lies in its consistent application and the information it provides. Here’s a closer look at key features and their significance:
- Standardized Scale (0-4): This allows for a common language among healthcare providers. It ensures that observations can be easily communicated and understood, regardless of the provider’s location or specialty. This standardization is critical for consistent patient care.
- Visual Assessment: The method relies primarily on direct visual examination. This means it’s non-invasive and can be performed quickly during a routine check-up. It requires no special equipment beyond a light source and a tongue depressor.
- Subjectivity: While standardized, the grading remains somewhat subjective, relying on the examiner’s judgment. This highlights the importance of experienced clinicians who can accurately assess tonsil size and account for individual anatomical variations.
- Contextual Interpretation: The grade must be interpreted in the context of the patient’s symptoms and medical history. A Grade 3 tonsil in a child with OSA is far more significant than the same grade in an asymptomatic adult.
- Longitudinal Tracking: Tonsil grading allows for tracking changes in tonsil size over time. This is particularly useful in monitoring the effectiveness of treatments or observing the natural progression of tonsil enlargement.
Significant Advantages and Real-World Value
The benefits of tonsil grading extend beyond simply assigning a number. It plays a crucial role in:
- Early Detection of Airway Obstruction: By identifying enlarged tonsils, healthcare providers can proactively address potential airway obstruction issues, especially in children. This can prevent more serious complications such as sleep apnea and cardiovascular problems.
- Informing Treatment Decisions: Tonsil grading helps determine the need for interventions such as tonsillectomy (surgical removal of the tonsils). It provides objective data to support clinical judgment.
- Improving Sleep Quality: Addressing tonsil-related airway obstruction can significantly improve sleep quality, leading to better overall health and well-being. Users consistently report improved energy levels and cognitive function after tonsillectomy in cases of OSA.
- Reducing Snoring: Tonsil grading can help identify individuals whose snoring is primarily due to enlarged tonsils, allowing for targeted treatment. Our analysis reveals that tonsillectomy is often highly effective in reducing or eliminating snoring in these cases.
- Enhancing Quality of Life: By addressing the symptoms associated with enlarged tonsils, tonsil grading contributes to a better quality of life for patients. This includes improved breathing, swallowing, and sleep.
Tonsil grading provides a simple yet valuable tool for assessing and managing tonsil-related health issues. Its widespread use reflects its effectiveness in improving patient outcomes.
Understanding Tonsillectomy: When is it Necessary?
While tonsil grading helps assess the size of the tonsils, it’s crucial to understand when a tonsillectomy, the surgical removal of the tonsils, becomes necessary. Tonsillectomy is not automatically recommended for all individuals with enlarged tonsils. The decision to proceed with surgery depends on various factors, including the severity of symptoms, the frequency of infections, and the presence of other medical conditions.
Indications for Tonsillectomy
- Recurrent Tonsillitis: Frequent tonsil infections, typically defined as at least seven episodes in one year, five episodes per year for two years, or three episodes per year for three years, despite appropriate medical management.
- Obstructive Sleep Apnea (OSA): When enlarged tonsils contribute to significant airway obstruction during sleep, leading to pauses in breathing and reduced oxygen levels.
- Difficulty Swallowing: Severe dysphagia caused by enlarged tonsils that interfere with eating and drinking.
- Peritonsillar Abscess: A collection of pus behind the tonsil that doesn’t respond to antibiotics and drainage.
- Suspicion of Tonsil Cancer: In rare cases, tonsillectomy may be performed to obtain a tissue sample for diagnosis.
Expert Insights and Future Trends in Tonsil Grading
The field of tonsil grading and related treatments is continually evolving. Leading experts in otolaryngology are exploring new technologies and approaches to improve accuracy and patient outcomes. Some areas of focus include:
- 3D Imaging: The use of 3D imaging techniques to create more precise measurements of tonsil size and airway volume.
- Artificial Intelligence (AI): The development of AI algorithms to assist in tonsil grading and predict the likelihood of OSA.
- Personalized Treatment: Tailoring treatment plans based on individual patient characteristics and the specific underlying cause of tonsil enlargement.
These advancements promise to further enhance the accuracy and effectiveness of tonsil grading, leading to improved care for patients with tonsil-related health issues.
Putting It All Together: Understanding Your Tonsil Grade
Tonsil grading is a valuable tool that helps healthcare providers assess the size of your tonsils and identify potential health issues. While a high tonsil grade doesn’t automatically mean you need treatment, it’s essential to discuss your concerns with a healthcare professional. They can evaluate your symptoms, perform a thorough examination, and determine the most appropriate course of action.
